National Guidelines for Family Centered Care in Phototherapy
Note: This guideline is currently under review.
Introduction
Aim
Definition of Terms
Cess
Managment
Potiential Complications
Belch Planning
Family Centered Care
Special Considerations
Companion Documents
Links
Bear witness Tabular array
References
Introduction
This guideline applies to neonates within the first two weeks of life.
Phototherapy is the use of visible low-cal to care for severe jaundice in the neonatal flow. Approximately threescore% of term babies and 85% preterm babies will develop clinically apparent jaundice, which classically becomes visible on day three, peaks days five-7 and resolves by 14 days of age in a term infant and past 21 days in the preterm babe. Treatment with phototherapy is implemented in order to prevent the neurotoxic furnishings of high serum unconjugated bilirubin. Phototherapy is a prophylactic, constructive method for decreasing or preventing the rise of serum unconjugated bilirubin levels and reduces the need for exchange transfusion in neonates.
Aim
This guideline provides health intendance providers with information to understand the causes of neonatal jaundice, the rationale for the use of phototherapy and outlines the care of neonates receiving phototherapy in gild to enhance constructive phototherapy delivery and minimise complications of phototherapy.
Definition of Terms
- Jaundice: the yellow appearance of the skin that occurs with the deposition of bilirubin in the dermal and subcutaneous tissues and the sclera.
- Bilirubin: the orange-xanthous pigment of bile, formed principally by the breakdown of haemoglobin in red claret cells at the end of their normal life-bridge. Neonate's bilirubin product rate is double that of adults and their clearance of bilirubin is reduced, hence the importance of monitoring levels and detecting jaundice in this early postal service-natal period.
- Bilirubinaemia: the presence of bilirubin in the blood.
- Hyperbilirubinaemia: the excess of bilirubin in the blood. Types of Neonatal Hyperbilirubinaemia:
- Unconjugated: most common grade of neonatal hyperbilirubinaemia. The bilirubin has not been metabolised and hence cannot be excreted via the normal pathways in the urine and bowel. Unconjugated bilirubin binds with lipids and albumin, and results in the xanthous advent of the skin and sclera. Unconjugated bilirubin tin cantankerous the blood-brain barrier and cause neurotoxic effects.
- Conjugated: less mutual in neonates. The bilirubin has been metabolised and is water soluble, only accumulates in the blood normally due to hepatic dysfunction. Conjugated bilirubin does not cantankerous the blood-brain barrier.
- Serum Bilirubin (SBR): reports the unconjugated and conjugated bilirubin levels. This is the usual specimen requested by Medical staff on the pathology sideslip at RCH. Hyperlink to RCH Specimen Collection handbook.
- Total serum bilirubin levels (TSB): measure used when charting serum bilirubin results onto Phototherapy and/or Commutation transfusion charts. TSB is the sum of unconjugated + conjugated serum bilirubin. A TSB can be requested on the pathology slip at RCH, merely just the total combined conjugated and unconjugated bilirubin level is reported.
- Breast milk jaundice: develops within 2-4 days of birth, is most likely related to limited fluid intake as breast milk supply is established, may summit at 7-15 days of age and may persist for weeks.
- Phototherapy: a handling for jaundice where the exposure of skin to a light source converts unconjugated bilirubin molecules into water soluble isomers that can be excreted past the usual pathways. Blue-dark-green light is most constructive for phototherapy every bit information technology both penetrates the pare and is absorbed by bilirubin to have the photochemical upshot.
- Bilirubin encephalopathy: the astute manifestations of bilirubin toxicity seen in the outset few weeks later on birth. Signs include lethargy, hypotonia and poor suck progressing to hypertonia, opisthotonos, loftier-pitched cry and eventually to seizures and coma.
- Kernicterus: the pathogenic diagnosis characterised past bilirubin staining of the brain stem and cerebellum. Besides the term used to refer to chronic bilirubin encephalopathy. Clinical findings include cognitive palsy, developmental and intellectual delay, hearing deficit, dental dysplasia and oculomotor disturbances.
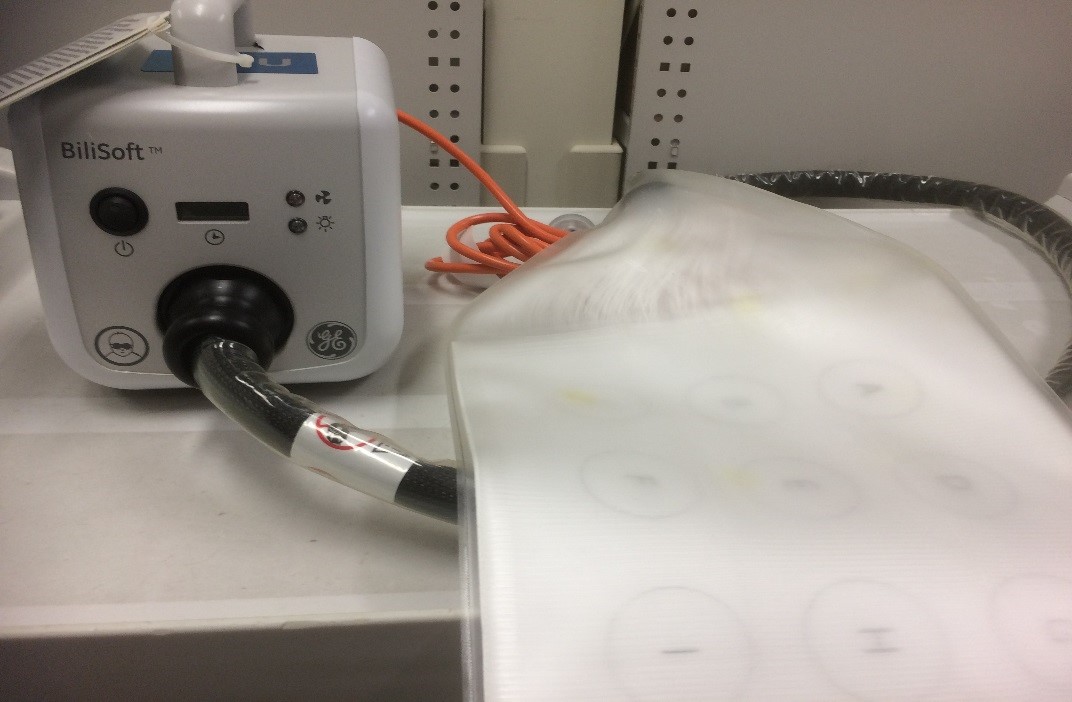
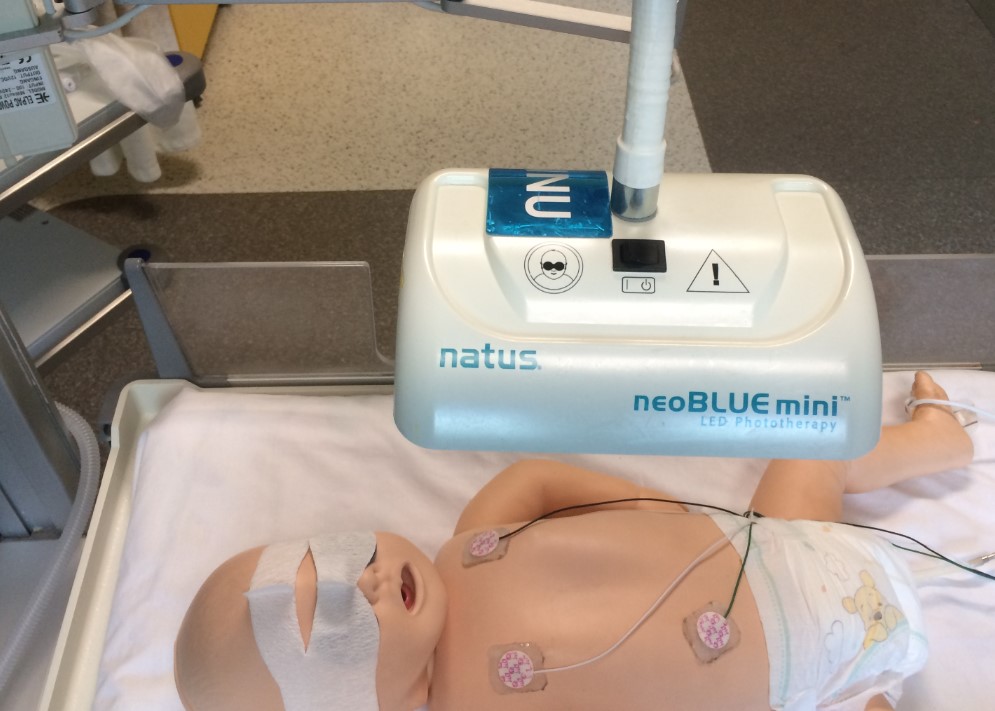
- Unmarried Light: One neoBLUE LED phototherapy unit (mini or standard)
- Double Lights: Ii neoBLUE LED phototherapy unit's (mini or standard) or 1 neoBLUE LED phototherapy unit (mini or standard) + One biliblanket
- Triple Lights: Iii neoBLUE LED phototherapy unit's (mini or standard) or 2 neoBLUE LED phototherapy unit (mini or standard) + One biliblanket
**All phototherapy units are to be ready on high intensity at all times, regardless of the amount of units in use. This ensures delivery of acceptable amounts of bluish light via light emitting diodes (LEDs). Therefore, a single unit of measurement is classified as a single light and unmarried, double or triple lights refers to the amount of units not the intensity setting.
**Equally per Natus neoBLUE LED phototherapy in-service guide (available on the intranet), mini neoBlue LED phototherapy units deliver the same intensity as the standard unit of measurement assault loftier intensity; the only departure is in the surface surface area coverage.
Assessment
Please annotation that when charting the TSB level onto the Phototherapy or Exchange Transfusion charts, in the presence of risk factors (sepsis, haemolysis, acidosis, asphyxia, hypoalbuminaemia) TSB values should be plotted on the range 1 lower than the neonate's gestational historic period/weight. This is because the risk of developing kernicterus increases in the presence of the to a higher place risk factors.
The Phototherapy and Exchange Transfusion charts onto which total SBR is plotted are for the first vii.5 and five days of life respectively. After the first five-7 days keep utilising these charts, equally levels plateau and tin keep to be documented.
- Assess general skin colour whenever measuring and recording vital signs. Ensure the Phototherapy tick box in the EMR Flowsheets is activated and document time of commencement and cessation.Obtain blood sample to measure out total serum bilirubin levels (either venous, arterial or capillary)
- Document hourly the type and number of calorie-free banks and the presence of eye protection.
- Obtain blood sample to measure full serum bilirubin levels (either venous, arterial or capillary) Hyperlink to RCH Specimen Collection handbook) Ensure the lights are turned off during sampling so accuracy of current blood levels can exist attained. Initially SBR levels may need to be assessed every 4-6 hours until reduction. Follow medical communication and ordering of SBR levels according to acuity of levels and plot on advisable line of the chart. Observe for signs of lethargy and poor feeding (insert link to assessing for Jaundice)
- Observe for signs of lethargy and poor feeding (insert link to assessing for Jaundice)
During phototherapy neonates require ongoing monitoring of:
- adequacy of hydration (urine output) and diet(weight proceeds)
- temperature
- clinical improvement in jaundice
- TSB or SBR levels
- potential signs of bilirubin encephalopathy
Investigations
- Initial TSB/SBR measurement should exist requested based on clinical observation and the following factors:
- any neonate <24 hours age with clinically apparent jaundice
- any neonate where in that location is clinical dubiety about the degree of jaundice
- any unwell neonate with jaundice
- whatsoever neonate with risk factors for jaundice (ABO/ Rh incompatibility, sepsis, acidosis, asphyxia, hypoalbuminaemia)
- Ongoing TSB/SBR measures should be repeated at intervals depending on the initial level and rate of ascent. For example: vi hourly measures may be required if the level is very high and the neonate is being treated with multiple phototherapy lights.
- A TSB/SBR may exist requested within 24 hours of ceasing phototherapy to assess for rebound hyperbilirubinaemia. Neonates at increased take chances of clinically pregnant rebound hyperbilirubinaemia include those born less than 37 weeks gestation, those not feeding optimally or those with haemolytic illness.
- Further Bloods and investigations include
- Maternal and infant blood type
- Direct Coombs test
- Haemoglobin
- Full blood count for red cell morphology; reticulcyte, haematocrit and platelet counts and white blood cell differential
- Urinalysis for reducing substances
- Sepsis screen if sepsis suspected
- G6PD and galactosaemia screens if suspected
- Serum thyroxine and thyroid-stimulating hormone levels
Risk Factors
- Mothers with a positive antibiotic screen
- A family history of G6PD deficiency
- A previously affected sibling
- Cephalhaematoma, bruising and trauma from instrumental birth
- Delayed passage of meconium
- Prematurity
- Dehydration
- Inadequate breastfeeding
- ABO incompatibility
- Rh incompatibility
Management
(link to phototherapy management certificate)
Nutrition
Breastfed babies who require phototherapy should continue to breastfeed unless clinically contra-indicated due to other pathology; the neonate'due south sucking, attachment and mother's milk supply should be monitored. In the case of infants nearing exchange transfusion level, the infant should not come out of phototherapy to feed as this is a medical emergency. All feeds should be given via a bottle or NGT if feeding is deemed safe
Neonates who are receiving enteral feeds of EBM or infant formula should continue to do then. The total fluid intake (TFI) for a 24 60 minutes catamenia may need to be increased by at least x% to account for insensible fluid loss when a neonate is receiving phototherapy however this should be guided by hydration condition and electrolyte monitoring.
Parenteral nutrition and IV fluids should continue as ordered and may also demand to be increased past 10% to account for insensible fluid loss.
Phototherapy
- Commence phototherapy once TSB/SBR is greater than the appropriate reference range for neonate'southward gestation/weight and presence of adventure factors.
- Neonates should be nursed naked autonomously from a nappy under phototherapy and will need to be nursed in an Isolette to maintain an appropriate neutral thermal surround. (Link to:" Ward Management of a Neonate" and "Isolette employ in Paediatric Wards") In astringent cases, the nappy may demand to be removed and a urine bag practical to maximise skin exposure.
- Positon phototherapy units no more than thirty.5cm from the patient. neoBLUE® LED phototherapy unit can be positioned as shut equally 15cm to patient. Refer to specific phototherapy units manufacturing guidelines for more details
- Expose as much of the skin surface equally possible to the phototherapy light. To maximise pare exposure, apparel the baby in a nappy and their protective eye covers only.
- Cover the eyes with appropriate opaque eye covers e.g. Natus Biliband® Eye Protector (bachelor from Butterfly ward).
- Ensure heart covers are removed 4-6 hourly for eye intendance during baby cares or feeding. Observe for belch/infection/damage and certificate any changes.
- Daily fluid requirements should be reviewed and individualised for gestational and postnatal age.
- Maintain a strict fluid balance chart.
- Chest feeds may need to be limited to 20 minutes if bilirubin level is high to minimise amount of time out of the lights
- Monitor vital signs and temperature at to the lowest degree 4 hourly, more oft if needed
- Encompass lipid lines with low-cal resistant, reflective tape to avoid peroxidation
- Ensure that phototherapy unit is turned off during collection of claret for TSB/SBR levels, as both conjugated and unconjugated bilirubin are photo-oxidized when exposed to white or ultraviolet light.
- Observe for signs of potential side effects.
Potential Complications
- Overheating – monitor neonate's temperature
- Water loss from increased peripheral blood menstruum and diarrhoea (if nowadays)
- Diarrhoea from abdominal hypermotility
- Ileus (preterm infants)
- Rash
- Retinal impairment
- 'bronzing' of neonates with conjugated hyperbilirubinaemia
- Temporary lactose intolerance
Belch planning and community-based management
Documentation in the neonates discharge letter and Child Wellness Booklet should include details near TSB/SBR levels and elapsing of phototherapy treatment.
Family Centered Care
Explain to parents the demand for and actions of phototherapy, particularly in relation to the need for skin surface to be exposed to the phototherapy lite, and hence the demand to care for neonates receiving phototherapy to exist nursed in a neutral thermal surroundings. Potential complications of phototherapy and the need for protective eye coverings during phototherapy handling should exist explained. The need for measuring the TSB and need for blood sampling should also exist explained.
Neonates receiving phototherapy (where there are no other contraindications) can have brief periods where the phototherapy is ceased so that they tin be cuddled/breastfed and have their eye covers removed for parent-baby interaction to occur.
Special Considerations
Normal hand hygiene measures should be attended to during intendance of a neonate receiving phototherapy.
More details on the neoBLUE LED lights can be plant in the definition of terms.
Companion Documents
- RCH Phototherapy Trial Chart - COMING Shortly
- RCH Exchange Transfusion Chart
- RCH Phototherapy competency
- RCH: Neonatal Clinical Practice Guideline: Exchange Transfusionhttp://world wide web.rch.org.au/uploadedFiles/Main/Content/neonatal_rch/EXCHANGE_TRANSFUSION.pdf
- RCH Clinical Do Guideline: Jaundice in early infancy http://www.rch.org.au/clinicalguide/guideline_index/Jaundice_in_Early_Infancy/
- RCH Clinical Guideline (Nursing): Ward Management of a Neonate http://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Ward_Management_of_a_Neonate/
- RCH Policy: Isolette use in Paediatric Wardshttp://world wide web.rch.org.au/policy/policies/Isolette_Use_in_Paediatric_Wards/
Links
- http://www.overnice.org.uk/
- http://www.overnice.org.uk/guidance/CG98
- http://pathways.squeamish.org.u.k./
- National Heart for Wellness and Care Excellence Pathways;
- Neonatal Jaundice (2014)
- Neonatal Phototherapy (2014)
- Neonatal jaundice single phototherapy (2014)
- Neonatal jaundice multiple phototherapy (2014)
- http://www.health.vic.gov.au/neonatalhandbook/
- https://thewomens.r.worldssl.net/images/uploads/fact-sheets/Jaundice-new-born.pdf
-
http://www2://health.vic.gov.au/hospitals-and-health-services/patient-intendance/perinatal-reproductive/neonatal-ehandbook/atmospheric condition/jaundice (2015)
Evidence Tabular array
Click here to view the evidence table for this guideline.
References
- Bhutani, V.K. and the Commission on Fetus and Newborn (2011) Phototherapy to prevent severe neonatal hyperbilirubinaemia in the newborn infant 35 or more weeks gestation, Pediatrics 128(4); e1046e1052
- http://www.wellness.vic.gov.au/neonatalhandbook/comditions/jaundice-in-neonates.htm retrieved 12/06/14
- Maisels, G.J. & McDonagh, A.F. (2008) Phototherapy for neonatal jaundice, New England Journal of Medicine 358(9): 920-928
- Neonatal Hyperbilirubinaemia, retrieved from
- http://www.merckmanuals.com/professional/pediatrics/metabolic_electrolyte_and_toxic_disorders_in_neonates/neonatal_hyperbilirubinemia.html 16/01/2014
- Overnice clinical guideline 98 (2010) Neonatal Jaundice, guidance.nice.united kingdom/cg98
- Queensland Maternity and Neonatal Clinical Guideline Neonatal Jaundice: prevention, assessment and management, Queensland Government (2009)
Delight remember to read the disclaimer.
The development of this nursing guideline was coordinated by Jessica Smith, Clinical Nurse Educator, Butterfly, and approved by the Nursing Clinical Effectiveness Committee. Updated Dec 2018.
Source: https://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Phototherapy_for_neonatal_jaundice/

0 Response to "National Guidelines for Family Centered Care in Phototherapy"
ارسال یک نظر